Internal Medicine Residency
Educational Experiences
Main navigation
At Iowa, we are dedicated to providing case-based, framework-focused didactic sessions and workshops that helps to supplement and accelerate our residents’ growth as clinicians. We do this through a variety of educational environments and distinct curricula.
We also currently offer two pathways and three distinction tracks (with hopes of adding more in the future) that give residents the opportunity to individualize their education and explore topics that interest them in a more in-depth manner.
Please explore the variety of learning environments, curricula, pathways, and distinction tracks we offer at the University of Iowa.
For information on research opportunities while in residency, visit the “Residents as Scholars” section.
Jump to: Learning Environments | Distinction Tracks | Pathways | Curricula
Highlights
Learning Environments
Learning Environments
All didactic sessions take place on a regular schedule that all faculty are aware of. This facilitates residents getting to conference on time and having a dedicated time for teaching in their daily schedules.
Noon Conference
From 12:00-1:00pm every Monday, Tuesday, Wednesday, and Friday (Thursday is Grand Rounds), all internal medicine residents and prelims on IM rotations gather in our lecture room for a didactic session. See the curricula below to see examples of what we learn about.
FREE FOOD IS PROVIDED! You don’t even have to use your call money. Noon conference time is a break in the day dedicated to learning where your time is protected, and you are only expected to respond to urgent messages.
While you are in the food line is a great time to socialize with your co-residents.
Morning Report
Morning report is led by residents for residents Every Wednesday from 7:15-7:45, a resident presents a case to the other residents on elective rotations to hear a case presentation. Chief residents help add to the teaching points brought up by the resident presenter.
Recent morning report cases:
- Fanconi syndrome due to oxaliplatin
- Discussion point 1: Physical exam findings to differentiate venous stasis from lymphedema
- Discussion point 2: Differentiating between the RTA type 1, 2, and 4
- Native-valve endocarditis leading to hemorrhagic stroke and altered mental status
- Discussion point 1: Framework for altered mental status
- Discussion point 2: Physical exam findings of endocarditis
- Air embolism leading to chest pain and stuttering speech
- Discussion point 1: Framework for chest pain in a patient with cancer
- Discussion point 2: Prevention and management of air embolism
Academic half day
On Thursday’s from 1:00-5:00pm on residents’ Y-week, residents participate in a variety of interactive didactic sessions. Depending on the week, residents will either be participating in the Ultrasound curriculum, RRT/Code blue simulation curriculum, Quality Improvement curriculum, Resident teaching skills curriculum, or Board review.
Additionally, each academic half day ends with an ambulatory workshop. The ambulatory workshop is an interactive session on a topic particularly relevant to primary care.
Topics covered recently include:
- Shoulder MSK physical exam and practicing shoulder injections
- Knee and ankle MSK physical exam and practicing knee injections
- Men’s health – BPH, ED, hypogonadism
- Women’s health – breast cancer screening and common breast problems
- LGBTQ+ health, health inequities, implicit bias
- Motivational interviewing for addressing substance use and obesity
- Anorectal disease and practice anoscopy
- Dermatology basics and practice skin biopsy
Master clinician rounds
Every Friday, from 8:00-8:30 the long call team presents one of their patients that they currently have on service to a master clinician (AKA our program director Dr. Suneja) and the chief residents, none of whom know the final diagnosis. As the case unfolds, the master clinician discusses their thought process as it applies to the case. After the presentation, the team and master clinician examines the patient and demonstrates relevant physical exam findings.
Internal Medicine Grand Rounds
On Thursday from 12:00 – 1:00, the whole internal medicine department gathers for grand rounds. Grand rounds are organized by the department of internal medicine. Topics are often focused to updating primary care providers and general internists to developments in the subspecialties.
Food is provided to all attendees, including residents!
Recent talks include:
- “Updates in Alcohol” by Dr. Andrea Weber
- “Osteoporosis in Patients with Anorexia Nervosa” by Dr. Amal Shibli-Rahhal
- “Rural Health: What it means for the VHA, UIHC, and the Nation” by Dr. Peter Kaboli
- “Death from Asthma” by Drs. Gregory Schmidt, Eyas Azayadneh, and Zeke Quittner-Strom (an internal medicine resident!)
Distinction Tracks
Our residency offers three distinction tracks that expand upon content that is taught in other parts of our residency’s curriculum. These distinction tracks meet on a monthly basis during the noon hour and discuss topics relevant to their distinction.
A crucial aspect of each of the distinction tracks is mentorship and a scholarly project. Scholarly projects give residents an avenue to apply what they learn in the distinction track meetings and mentors identified through the distinction track provide regular guidance.
Pathways
Our residency offers two pathways that are tailored to residents interested in primary care or hospitalist medicine.
Primary Care Pathway
The Primary Care Pathway is a flexible program designed to provide clinical experiences and education that support residents in the pursuit of excellence in primary care. As part of the pathway, residents are invited to attend educational sessions over the noon conference hour that focus on different aspects of primary care like the similarities and differences between community and academic primary care, billing in primary care, and how to go about a job search for primary care physicians. Residents in the primary care pathway are given scheduling priority for rotations that prepare them for primary care like sports medicine, dermatology, women’s health, and the Medication-Assisted Treatment (MAT) clinic. Residents are also paired with a mentor who shares similar interests and career goals to help them as they work through this pathway.
Hospitalist Pathway
The Hospitalist Pathway is designed for residents who wish to prepare for a career in inpatient general medicine. As part of this pathway, residents are given priority in scheduling career specific rotations like the stroke team and the hospitalist elective, which is a one-on-one experience with an experienced hospitalist on a non-teaching service. Residents also attend conferences hosted over the noon hour where hospitalists discuss topics like inpatient billing, health care delivery systems, patient safety, and how to go about doing a job search for hospitalist positions with the residents.
Curricula
Core Topics in Internal Medicine
The majority of noon conference topics fit under this curriculum. We emphasize having a curriculum that is interactive and case based. We cover topics from all subspecialties of internal medicine (and beyond) that are relevant for general internists and primary care doctors.
Highlights from this series include:
- The “Emergencies” lectures: Infectious disease emergencies, endocrine emergencies, dermatologic emergencies, and psychiatric emergencies to name a few
- “Pancreatic cystic lesions”
- “Buprenorphine 101”
- “Breast cancer for the internist”
- There are also disease focused talks, like “Acute pancreatitis” and “Chronic Obstructive Pulmonary Disease” other important talks like that
Ultrasound Curriculum
The Point-of-Care Ultrasound (POCUS Curriculum) is a longitudinal, integrated, and progressive learning experience that teaches bedside ultrasonography and how it can be utilized in patient care. This curriculum is taught during the academic half day of the Y-week. This curriculum focuses on hands-on scanning of simulated patients with in-person faculty mentors who provide real-time feedback.
Here are some example modules:
| Basic POCUS Modules (PGY-1) | Advanced POCUS Modules (PGY-2 and above) |
|---|---|
|
|
Quality Improvement curriculum
The Quality Improvement curriculum at the University of Iowa is an integrated curriculum that incorporates workshops during the academic half day of the Y week and a year-long team-based quality improvement project designed and implemented by the Y week cohorts.
University of Iowa Health Care hosts an annual Quality and Safety Symposium in which our resident teams are given the opportunity, encouragement, resources, and mentorship to submit and present their projects. After this, many teams submit their projects to large regional and national meetings.
Since the development of our curriculum we have had…
- 50+ resident led QI Projects
- 30+ resident led QI Projects presented at our local Quality and Safety Symposium
- 25 resident teams presented oral presentation or posters at SGIM Midwest Regional Meeting
- 7 resident teams presented posters at SGIM National Meeting
Our groundbreaking curriculum was published in the Journal of Graduate medical Education.
Example QI projects:
- Naloxone prescription for opioid use disorder
- Hepatitis C screening
- Patient-Provider Communication – AVS summary use at the VA
- SGLT2 prescription for CKD
Clinical Reasoning curriculum
One of the highlights of our program’s curricula is the emphasis on clinical reasoning. Clinical reasoning is a unifying theme of all that we teach here at the University of Iowa. But clinical reasoning takes the spotlight during clinical reasoning week, where Dr. Suneja (our program director) and company take a deep dive into the inner workings of the thought processes of master clinicians. We discuss the nuts and bolts of problem representation and how to form an effective assessment. We then use that problem representation and show how that interacts with frameworks, which ultimately lead to a differential diagnosis. We also discuss cognitive bias and how clinicians are continuously learning and incorporate this new information into their thought processes.
Topics covered include
- “Clinical Reasoning: Thinking of blinking”
- “Speaking the same language and steps to clinical reasoning”
- “Clinical Reasoning: Novice to Expert”
Additionally, the primary focus of Morning Report, Master Clinician Rounds, Framework Friday’s, and Master Clinician Mystery Case series is clinical reasoning. All of these experiences work together to develop our residents clinical reasoning skills over their three years of residency.
Framework Fridays
Introduced in 2023, Framework Friday’s are case presentations led by the chief residents during noon conference that dive deeply into a framework and how applies to clinical reasoning related to the case.
Topics covered include:
- Shortness of breath
- Hemolytic anemia
- Microcytic anemia
Master Clinician Mystery Case Series
The Master Clinician Mystery Case Series was developed by residents Luke Morrey and Rachel Genova (’23) as part of a Distinction in Medical Education (link) curricular project. For this series, a case is presented to a master clinician in aliquots and the attendees break into small groups and discuss their approach to the case before coming back as a group to hear what the master clinician is thinking as the case unfolds. The emphasis is on reasoning and the correlation between basic pathophysiology and clinical presentation.
Topics covered include:
- Pulmonary-renal syndrome
- Lactic acidosis
- Interstitial Lung Disease
RRT/Code Blue simulation
Residents participate in simulations of Rapid Response and Code Blues during the ambulatory curriculum of their Y week. This is a progressive learning experience with the PGY2s running the simulation, the PGY1s assisting and the PGY3s giving feedback. This was an addition to the educational opportunities made available to residents during the 2023-2024 academic year and it has been very well received.
Board Review curriculum
Board review is a longitudinal curriculum that occurs during the academic half day of Y weeks and during noon conference in the later part of the year. Additionally, our program facilitates a “Board Review Weekend” at the end of the academic year for graduating residents. These didactic sessions are organized around MKSAP questions and focused on content heavily covered by the ABIM in order to reinforce clinical reasoning, key points, and test taking strategies.
Resident Teaching Skills curriculum
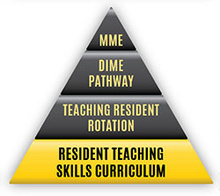
The Teaching Skills Curriculum is a longitudinal, integrated, and progressive workshop-based curriculum that introduces residents to the knowledge base and skill set used when serving in the role of a clinician-educator. This curriculum is taught during the academic half day of the Y-week. This curriculum focuses on skills and techniques that would be used to teach medical students while on rotations like creating an effective learning climate, one-minute preceptorship, and chalk-talk 101.
Teaching Skills Curriculum Goals

- Teaching Skills Curriculum Goals
The goal of the Teaching Skills curriculum is to introduce residents to a knowledge base and skill set used when serving in the role of a clinical educator. The longitudinal curriculum for all residents presents concepts and allows residents to practice skills associated with topics such as establishing the learning climate, motivating the learner, one-minute preceptor and feedback and evaluation as well as interactive teaching and evaluation.
Sessions are interactive covering a topic related to current best teaching practices. There is time for skill development and through the process of deliberate practice, residents design an action plan for further skill development. Residents complete pre-session readings and following each session are expected to refer to their action plan in teaching encounters.
Session #1: Introduction to Teaching Skills, Learning Climate and Effective Teachers
- identify characteristics of exemplary clinical teachers
- identify strategies to promote an effective learning climate
- demonstrate teaching behaviors that promote an effective learning climate
- develop an action plan to improve the learning climate in your own teaching
Session #2: Motivating the Learner
- examine contributing factors that affect a learner’s performance.
- explain one relevant motivational theory that covers extrinsic & intrinsic motivators.
- discuss the importance and impact of a good orientation.
- identify components of an orientation.
Session #3: One-Minute Preceptor
- describe the 5 elements of the one-minute preceptor model for clinical teaching.
- successfully apply the model to a simulated learner presenting a patient.
- use the model to develop an assessment of the learner’s current level of knowledge/skill and what the learner needs to know.
Session #4: Feedback
- define feedback and give rationale for providing feedback to learners.
- recognize barriers to giving feedback.
- identify characteristics of effective feedback.
- demonstrate effective feedback via observation and practice.
- develop an action plan for improving personal feedback skills.
Session #5: Interactive Teaching/Use of Technology
- know the goals of effective lecturing/presentation.
- describe components of effective lecturing/presentation.
- apply specific techniques for making lectures more interactive.
Session #6: Evaluation of Students, Peers and Faculty
- define evaluation and differentiate it from feedback.
- obtain an understanding of the use of commonly used evaluation tools and techniques.
- gain insight into common pitfalls surrounding evaluations.
- understand why accurate evaluation is important.
Wellness curriculum
The wellness curriculum covers a wide spectrum of issues related to wellness. The talks are selected and organized by the Wellness and Humanities Committee. Some of the favorite talks from this series are the yearly two-part talk on personal finance and the faculty panel on dealing with errors.
Wellness talks during noon conference include:
- “Sleep during residency”
- “Financial wellness” – a 2 part lecture series
- Faculty panel on dealing with errors and patient death
- Our yearly Pumpkin Carving Contest and Holiday party with cookie decoration that happen over noon conference
Population Health curriculum
Introduced in spring of 2023, the purpose of the Population Health curriculum is to increase residents’ awareness of issues of health equity within medicine and give residents tools to minimize them. These talks are given during noon conference on a regular interval to increase our residents training in this critically important issue. For residents learning more about health inequities in medicine, we also offer a Distinction in Population Health as well as clinical experience in the Free Medical Clinic.
Talks given in this series include:
- “Health equity and disparity”
- “Stigma and evaluation in substance use”
R2 Talks
All second-year residents participate in creating and delivering a noon conference lecture and handout on an educational topic of their choice. Residents are paired with faculty mentors and given feedback.
Talks given by residents include:
- “Alcohol-associated hepatitis”
- “Infective endocarditis: beyond the TEE”
- “Pulmonary Langerhans Cell Histiocytosis”
- “Clinical diagnostic errors”
Journal Club
All third-year residents lead a discussion of a current primary literature in internal medicine or internal medicine subspecialties. There focus is on critically appraising the study design and evaluating the applicability of these results to patient care.